Stigma surrounding OCD stems from stereotypes and miseducation
Disclaimer: This article should not be used as a tool for diagnosis. If you are concerned that you may be experiencing symptoms of OCD, please talk to a parent, counselor or medical professional.
*Names changed for confidentiality
David Beckham. Leonardo DiCaprio. Katy Perry.
Although these celebrities do not appear similarly at a first glance, they have one thing in common: they have all publicly opened up about their struggles with obsessive-compulsive disorder.
Mayo Clinic describes OCD as “excessive thoughts that lead to repetitive behaviors.” These thoughts are also known as obsessions, and these behaviors are also known as compulsions, hence the name of the disorder.
Almost all forms of OCD incorporate obsessions and/or compulsions. But according to OCD UK, it is important to realize that these symptoms can manifest in different ways in different people.
“A lot of people think OCD is just about wanting a clean room and an organized pencil case,” junior Meghan Scott* said. “Mine is more about contamination and what touches what. My room and my pencils are a mess.”
While there are infinite forms of OCD, most cases tend to fall into one of five categories: checking, contamination, symmetry, ruminations, or repeated thoughts, and hoarding. Each subtype’s compulsions are typically caused by underlying obsessions. For example, a person experiencing contamination OCD may excessively wash their hands due to a hidden fear that not doing so could harm them or their loved ones. This is the case for junior Olivia Matthews*, who was diagnosed during seventh grade.
“I used to take over two hours to get ready for bed because I couldn’t stop repeating simple tasks,” Matthews said. “My nightly routine kept my family and I awake longer and longer each night, and it went on like that until I received treatment.”
Matthews began treatment directly after receiving her diagnosis. She visited multiple therapists over the course of the next year before deciding she needed a more vigorous treatment plan. She then worked with her parents to find a residential care facility at the beginning of her freshman year.
During her two and a half months at the facility, Matthews participated in exposure therapy. Exposure therapy creates a safe environment in which to “expose” people to their phobias in an attempt to overcome them.
Matthews’ exposure therapy first focused on low-anxiety phobias, or phobias inducing low levels of anxiety, such as touching door handles. Over time, she dealt with increasingly high-anxiety phobias, or phobias inducing high levels of anxiety, such as eating food off the floor after it had been stepped on. When she left the facility, many of her high-anxiety phobias had regressed into low-anxiety phobias, and many of her low-anxiety phobias had disappeared entirely.
“[After exposure therapy], I would have to sit down for a few minutes because I could hardly breathe,” Matthews said. “Now, when I’m struggling, I’m able to think back to what I went through during exposure therapy and what I did to get through it.”
Matthews continues to receive medication and attend weekly therapy sessions to discuss her progress. Although OCD is an incurable mental illness, therapy allows her to manage her symptoms and minimize their effect on her daily life. She encourages anyone experiencing similar symptoms to reach out to a trusted adult for help.
“I think a lot of teenagers are still embarrassed to talk to a professional about it,” school psychologist Jennifer Zacharski said. “They need to know that it’s a sign of courage to ask for help—not weakness.”
Speaking with a licensed psychologist or psychiatrist can also help prevent misdiagnosis, Zacharski said. After learning about a disorder, it is easy to compare its symptoms to personal experiences. A majority of people experience OCD-like tendencies, or thought processes commonly associated with OCD, leading to frequent self-diagnosis. Despite these tendencies, only approximately 1% of people experience the actual disorder, according to Teen Mental Health.
“We all obsess over things to a certain extent,” Zacharski said. “It’s completely normal to be worried about whether or not you turned off the stove or locked the back door. It only becomes a problem when it makes you late consistently to the point that it impairs your functioning.”
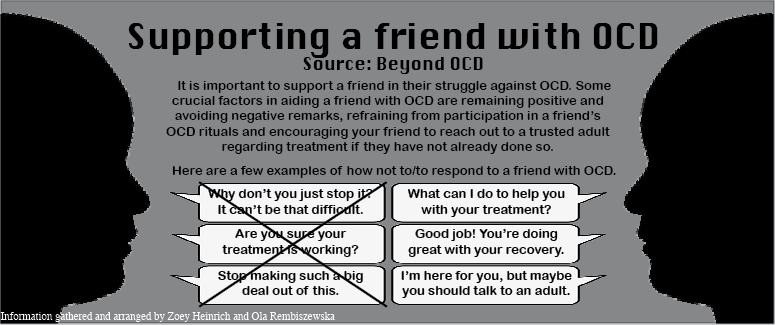
According to Zacharski, struggling with OCD as an adolescent can often lead to feelings of marginalization. The disorder does not usually receive as much media attention as other disorders such as anxiety and depression, causing stigma to surround it. Anyone can contribute to eliminating this stigma by researching the topic, disregarding stereotypes and encouraging the discussion of mental wellness with professionals, Zacharski said.
“You’re not crazy,” Scott said. “It’s easy to feel that way when no one completely understands what you’re doing or why you’re doing it, but you’re not crazy, and you deserve to get help just as much as anyone else does.”